
Heart failure is a clinical syndrome that is the end-stage manifestation of a variety of cardiac diseases. Subgroup analysis showed that MELD-XI score still had prognostic value in the subgroup without chronic kidney disease (HR 3.30 95%CI 2.01–5.42 P < 0.001 HR adjusted 1.88 95%CI 1.06–3.35 P = 0.032, P for interaction = 0.038).Ĭonclusions: This study proved that the MELD-XI score at admission was related to the poor prognosis of hospitalized patients with chronic heart failure within 3 years. Survival analysis results showed that elevated MELD-XI score at baseline predicted the risk of all-cause mortality at 3 years in patients (HR 3.19, 95% CI 2.11–4.82, P < 0.001 HR adjusted 1.79, 95% CI 1.09–2.92, P = 0.020). Six characteristic variables (NT-proBNP, BUN, RDW CV, Na + and prealbumin) were selected by univariate Cox regression and lasso regression. During the 3-year follow-up period, there were 97 all-cause deaths, including 63 cardiac deaths. Results: A total of 400 patients with chronic heart failure were included (median age 76 years, 51.5% female). Survival curves were estimated using the Kaplan–Meier method and compared by the log rank test. Combined with the MELD-XI score, the final model was adjusted, and the predictive ability of the model was evaluated. Cox regression and lasso regression were used to screen variables and build a prognostic model. The primary clinical outcome was all-cause mortality within 3 years. Methods: This is a retrospective cohort study of patients with chronic heart failure who were initially hospitalized in the Second Affiliated Hospital of Chongqing Medical University from February 2017 to December 2017. The aim of this study was to determine the long-term prognostic relationship of MELD-XI score in patients with chronic heart failure. Objectives: The relationship between the MELD-XI score, a modified version of the MELD score, and the long-term prognosis of hospitalized patients with chronic heart failure is unclear. 8Department of Cardiology, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China.7Department of Cardiology, The First Affiliated Hospital of University of Science and Technology of China, Hefei, China.6Department of Hepatobiliary Surgery, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China.5Department of General Medicine, The Second Affiliated Hospital of Chongqing Medical University, Chongqing, China.4Clinical Research Center for Respiratory Disease (tumor) in Anhui Province, Bengbu, China.3Anhui Province Key Laboratory of Clinical and Preclinical Research in Respiratory Disease, Bengbu, China.2Department of Pulmonary and Critical Care Medicine, First Affiliated Hospital, Bengbu Medical College, Bengbu, China.1Department of Geriatrics, Zhongshan Hospital Affiliated to Xiamen University, Xiamen, China.We demonstrate an evidence-based method to incorporate Na into MELD, which provides more accurate survival prediction than MELD alone.Zebin Lin 1 † Xia Liu 2,3,4 † Li Xiao 5 Yin Li 6 Chenlu Qi 5 Siqi Song 5 Yiping Zhao 7 Lili Zou 8 *

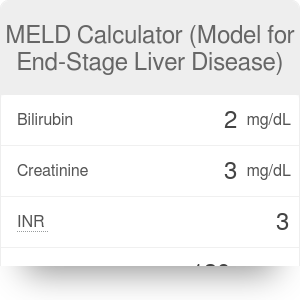
If this new score were used to allocate grafts, it would affect 27% of the transplant recipients. In this cohort, "MELD-Na" scores of 20, 30, and 40 were associated with 6%, 16%, and 37% of risk of death within 6 months of listing, respectively. A new score to incorporate Na into MELD was developed: "MELD-Na" = MELD + 1.59 (135 - Na) with maximum and minimum Na of 135 and 120 mEq/L, respectively. After adjustment for MELD score and center, there was a linear increase in the risk of death as Na decreased between 135 and 120 mEq/L. MELD score and Na, at listing, were significant (both, P <. During the study period, 67 patients (9%) died, 243 (32%) underwent transplantation, 73 (10%) were withdrawn, and 370 were still waiting. Low Na (<130 mEq/L) was present in 8% of patients, of whom 90% had ascites. Adult, primary liver transplant candidates with end-stage liver disease were enrolled.Ĭomplete data were available in 753 patients, in whom the median MELD score was 10.8 and sodium was 137 mEq/L. We evaluated methods to incorporate Na into model for end-stage liver disease (MELD), using a prospective, multicenter database specifically created for validation and refinement of MELD. Serum sodium (Na) concentrations have been suggested as a useful predictor of mortality in patients with end-stage liver disease awaiting liver transplantation.


 0 kommentar(er)
0 kommentar(er)
